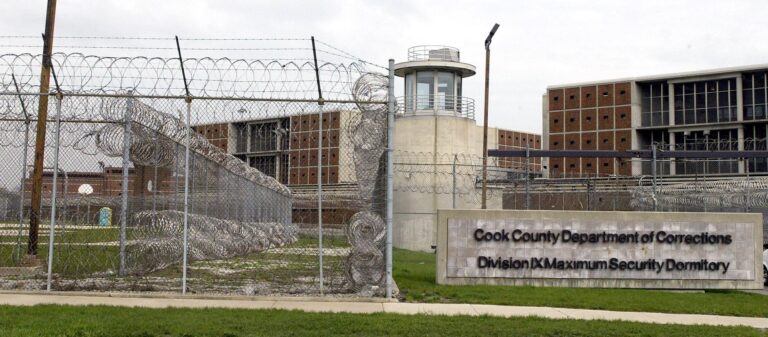
Chicago’s Cook County Jail: A Growing Mental Health Care Hub Amid Systemic Challenges
The Mental Health Emergency Within Chicago’s Overcrowded Jail System
Chicago’s Cook County Jail has increasingly become one of the nation’s largest providers of mental health services, underscoring a critical and often neglected overlap between the criminal justice system and public health care. Despite ongoing initiatives to bolster community-based mental health support, a significant portion of individuals with psychiatric disorders find themselves incarcerated, where access to adequate treatment remains severely limited.
The jail’s overcrowding intensifies this crisis, straining staff capacity and complicating efforts to deliver timely and effective care. Many inmates display symptoms ranging from intense anxiety and depression to severe psychosis, yet face prolonged delays before receiving any form of mental health intervention.
Key challenges confronting the jail’s mental health care include:
- Insufficient mental health personnel overwhelmed by the volume of cases
- Frequent shortages of psychiatric medications and limited therapeutic options
- Correctional officers often lack adequate training in managing mental health crises
- High recidivism rates linked to untreated or poorly managed mental illness
| Challenge | Consequences | Reported Frequency |
|---|---|---|
| Staffing Deficits | Delays in mental health assessments | Over 700 cases monthly |
| Medication Shortfalls | Worsening psychiatric symptoms | 450+ incidents reported |
| Overcapacity | Restricted treatment space | Average occupancy at 120% |
These systemic shortcomings highlight the urgent necessity for reforms both inside correctional institutions and within the broader mental health care infrastructure serving at-risk populations.
Rising Demand Overwhelms Inmate Mental Health Services
As the number of incarcerated individuals with mental health conditions continues to climb, Chicago’s jail system struggles to meet the growing demand for behavioral health services. Existing programs are stretched thin, resulting in extended wait times and limited availability of specialized care. Budget constraints and workforce shortages force administrators to make tough choices about resource allocation.
Primary obstacles in delivering inmate mental health care include:
- Shortage of qualified mental health clinicians: The counselor-to-inmate ratio falls well below recommended national guidelines.
- Facility overcrowding: Limited space hampers the ability to isolate and treat individuals experiencing acute crises.
- Fragmented care continuity: Transition plans linking jail-based treatment to community services are inconsistent and underfunded.
| Service | Current Capacity | Demand Growth (Past 2 Years) |
|---|---|---|
| One-on-One Counseling | 350 inmates weekly | +25% |
| Group Therapy Sessions | 150 inmates weekly | +30% |
| Crisis Response Availability | 24/7 coverage | +40% |
Advocating for Community-Centered Alternatives to Incarceration
In light of the overcrowding and mental health challenges within Chicago’s jails, experts increasingly call for a paradigm shift toward community-based interventions.These approaches focus on addressing underlying factors such as untreated psychiatric disorders and substance abuse by offering supportive, rehabilitative environments rather than punitive incarceration. Research shows that investing in community programs not only alleviates jail overcrowding but also improves long-term outcomes for individuals and society.
Highlighted community initiatives include:
- Crisis Intervention Teams (CIT): Collaborative units pairing law enforcement with mental health professionals to divert individuals from jail to appropriate treatment settings.
- Supportive Housing Programs: Providing stable residences coupled with counseling and healthcare services to promote recovery.
- Peer-Led Support Networks: Groups facilitated by individuals with lived experience to foster reintegration and sustained recovery.
| Program | Primary Focus | Measured Impact |
|---|---|---|
| Crisis Intervention Teams | Emergency mental health response | 40% reduction in jail bookings |
| Supportive Housing | Long-term stability | 30% decrease in recidivism |
| Peer Support | Community reintegration | Improved treatment adherence |
Transforming Mental Health Services to Reduce Jail Populations
Urban jail systems like Chicago’s have inadvertently become the default safety net for individuals experiencing severe mental health crises. A disproportionate number of inmates suffer from diagnosable psychiatric disorders, yet correctional facilities lack the resources and expertise to provide comprehensive care. Without significant reforms, experts warn that the cycle of incarceration and inadequate treatment will persist, placing increasing strain on the justice system.
Effective strategies to mitigate this crisis include:
- Expanding early intervention and community-based mental health programs.
- Enhancing intake screening to promptly identify inmates requiring psychiatric care.
- Strengthening collaboration among law enforcement, healthcare providers, and social service agencies.
Recent data highlights stark disparities between the jail population and the general public:
| Mental Health Indicator | Cook County Jail (%) | General Population (%) |
|---|---|---|
| Serious Mental Illness Diagnosis | 45% | 5% |
| Receiving Treatment at Intake | 12% | N/A |
| Reoffending Within One Year | 60% | N/A |
Looking Ahead: Addressing the Intersection of Mental Health and Incarceration
Cook County Jail’s role as one of the largest mental health care providers in the U.S. starkly illustrates the systemic failures in addressing mental illness outside the criminal justice system. The facility’s challenges reveal significant gaps in community-based treatment availability and underscore the pressing need for comprehensive reforms. While ongoing efforts aim to improve conditions, the jail remains a powerful symbol of how intertwined and under-resourced America’s justice and health systems are when it comes to supporting society’s most vulnerable individuals.